Individual Funding Requests
|
Important Notice
NHS Vale of York Clinical Commissioning Group has been dissolved and replaced by the NHS Humber and North Yorkshire Integrated Care Board (ICB) on 1 July 2022. Details of the arrangements for individual funding requests (treatment not routinely commissioned by the NHS) can be found on the ICB website.
The Integrated Care Board (ICB) has established a clinically and professionally led Group comprised of former CCG experts, which includes GPs representing each local area, to lead the review of all clinical policies. The group aims to prepare commissioning policies in two waves – wave one will be completed by the end of March 2023 and wave two by the end of March 2024.
Until the review is complete, the ICB has adopted an interim approach to Individual Funding Requests, using commissioning statements aligned to CCG areas as they were on 30 June 2022. More information can be found here. |
This page helps to describe how we make decisions about providing treatments which are not normally available through the NHS in this area.
Why does the CCG need to have an Individual Funding Request policy?
Every year the CCG receives money from the Government to pay for healthcare for everyone registered with a GP in the area. The NHS has limited resources, and we have a duty to manage them carefully. Demand for healthcare is growing. New and often expensive treatments are becoming available all the time. Our priority is to pay for those medicines and treatments that have good scientific evidence for their safety and effectiveness and offer good value for money.
As a result there are some treatments we do not normally pay for.
Our Individual Funding Request (IFR) policy sets out the principles behind our decisions on individual treatments. It also explains the system we have for processing each individual request for treatment.
This leaflet explains how your doctor, NHS Consultant, or other healthcare specialist (all referred to from now on as clinician) can ask us, on your behalf, to pay for a treatment that we do not normally fund. Click here to view this leaflet.
What happens if a treatment is not normally available?
Your clinician can make an Individual Funding Request (IFR) for either of two reasons:
- for treatment which is not routinely funded
- or for a treatment which is funded in line with specific criteria, which you do not meet.
For either of the above, funding can only be approved if a case of “exceptional clinical need” has been demonstrated.
What is “exceptional clinical need”?
A patient may be considered to be clinically exceptional to the general policy if both of the following apply:
• the patient is significantly different from the general population of patients with the condition in question and
• the patient is likely to gain significantly more benefit from the intervention than might normally be expected for patients with that condition.
It is important for patients to be aware that only evidence of clinical need will be considered. Factors such as gender, ethnicity, age, lifestyle or other social factors such as employment or parenthood will not be considered. The fact that the treatment might be effective for the patient is not, in itself, grounds for exceptionality.
The IFR process
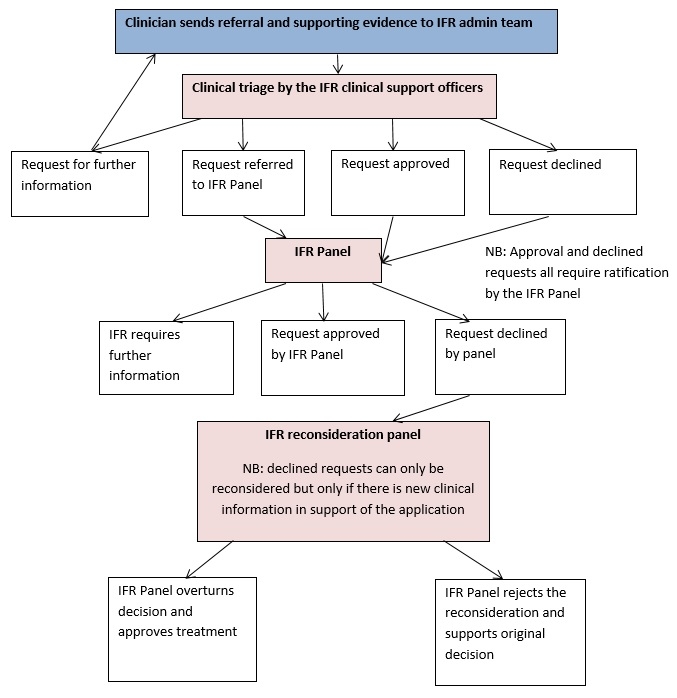
Your clinician will complete a referral form and forward it to the IFR Team along with any supporting clinical information. It is the responsibility of the requesting clinician to demonstrate why they feel your case may be suitable for individual funding.
What happens next?
Your application will be clinically triaged. That is, it will be assessed by the IFR Team, which includes a qualified Nurse specifically trained in the IFR process.
If there is not enough information provided, your case will be returned to your clinician for further supporting information.
If the request fulfils the IFR policy for your CCG, then your application will be approved. If the criteria have not been met and clinical exceptionality has not been sufficiently demonstrated, your application will be declined. If your application is more complex then it will be submitted to an IFR Panel.
How does an IFR Panel make decisions?
The IFR Panel consists of two CCG GPs who are supported by appropriate specialists who will assess the clinical information and evidence that your clinician has provided.
The Panel considers the application against set criteria laid down in the CCG’s commissioning policies and will support funding if exceptional clinical need has clearly been demonstrated.
What happens after the decision is made?
If your treatment is approved, your clinician will be informed of the decision in writing and will contact you to get your treatment underway.
If the funding request is declined, you will be informed directly in writing.
Having a Decision Reconsidered
Where a request for funding has been declined, the patient’s referring clinician has the opportunity to ask for the decision to be reconsidered. However decisions can only be reconsidered if there is new clinical information in support of the request.
Patients are not able to ask for a reconsideration directly themselves, the patient’s referring clinician must do this on the patient’s behalf.
Appealing the Process
An appeal only occurs if the referring clinician feels the IFR process has not been followed when dealing with the request.



