COVID-19 Vaccination FAQs
This page was last updated: 12/07/2021
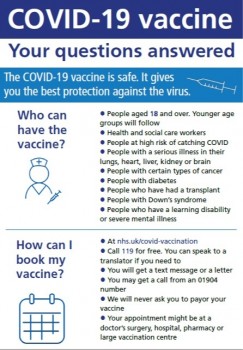
Download our COVID-19 FAQ leaflet here.
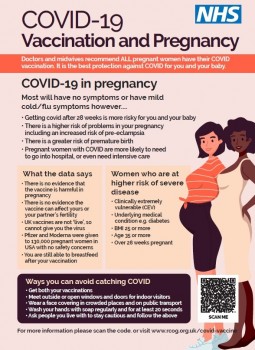
Download a guide to COVID-19 vaccination and pregnancy here
|
The national booking service is currently open to anyone who is:
If you are eligible to receive the COVID-19 vaccine, you can arrange a vaccination online or by telephone. Visit nhs.uk/covid-vaccination or call 119 (available 7 days a week, 7am-11pm). |
You don’t have to do anything. You will be contacted by the NHS and invited for a vaccine when the time comes. No one will be left out.
The invitation may be from your local GP surgery or a mass vaccination centre. If you receive an invitation from both, choose which is best for you. The nearest mass vaccination centre in our region is at York Askham Bar, Park and Ride.
If you receive an invitation to Askham Bar, you can choose to book an appointment there or, if this is not possible, you can wait to be invited to an appointment by your GP.
Read more about the NHS Vaccination Centre at Askham Bar, York.
There is a priority list setting out which people will be invited for a vaccination in which order. The initial priority groups to receive the vaccine are:
- Residents in care homes, and their carers
- People aged over 80
- Frontline health and social care workers
- People aged 75 and over
- People aged 70 and over and clinically extremely vulnerable individuals
You can learn more about who may be clinically extremely vulnerable here.
The priority list for vaccinations has been developed and is kept under review by the Joint Committee on Vaccination and Immunisation.
Yes. It is important that you receive the second dose of the vaccine when you are invited.
This ‘booster’ is an important part of the vaccination process and is common with many vaccines. The timing of second doses will be in line with the standard operating procedure for each vaccine, normally around 12 weeks after your first dose.
We will arrange your second dose with you, there is no need to call your GP to arrange.
You will have increased protection from serious illness caused by the COVID-19 between two and three weeks after your first dose of the vaccination.
However, it is important that everyone, including those who have received a vaccination, continues to comply with government guidance, including social distancing, face coverings and hand washing guidance.
Vaccinations are taking place at a blend of GP surgeries, hospitals, public vaccination sites and in care settings. We also expect additional locations will be developed. Your vaccination site will be clearly indicated when you receive your invitation from the NHS for your vaccination appointment.
People should access their vaccination appointment in the same way they would access any other medical appointment using existing services. In addition, if needed, there may be volunteer drivers available, charities are offering their support and patients who meet the criteria for patient transport for medical appointments may also be able to use that service.
We strongly encourage everyone who can to attend a vaccination site when invited. We are working through the best ways to bring the vaccine to those who are unable to leave their home as a healthcare system. How this will best be achieved is shaped by the characteristics of the vaccines available.
Each of the three vaccines now approved has undergone rigorous assessment by the UK regulators (the Medicines and Healthcare products Regulatory Agency).
Side effects caused by the vaccine are mild and are much less serious than developing the virus or complications associated with it. They usually go away within a few days.
There has been a very small number of people who have experienced an extremely rare event where blood clots developed after the first dose of the vaccine. These people were mainly under the age of 30 and research is going on to understand if the clots are directly cause by the vaccine. The Government says that an alternative vaccine should be offered to those under 40 years of age. The risks of getting clots from COVID far outweigh the risk of clots from the vaccine.
No, this is not possible. The vaccine ingredients can not enter the nucleus (the centre) of the cell, which means it is can not affect your DNA.
Bell’s palsy is a temporary weakness of the muscles in the face. We don’t know what causes it, but it might be an infection. Some people taking part in the Pfizer trial developed Bell’s palsy. It was a very small number and we do not think the vaccine caused it.
If you are pregnant, you will be offered the vaccine when it is time for your age group. Please speak to your doctor or midwife to make sure they are happy for you to have the vaccine. The vaccine can not give you or your baby COVID-19.
In later pregnancy, some women could become seriously ill if they have COVID-19. Pregnant women with COVID-19 are more likely to have to go into intensive care in hospital. Pregnant women with COVID-19 are more likely to have their babies early, and pregnant women are more at risk from COVID-19 if they have immune problems, diabetes, high blood pressure and asthma.
Pregnant women are more at risk from COVID-19 if they are overweight, older than 35, more than 28 weeks into their pregnancy, or are of black or Asian ethnic minority background.
There have been no safety concerns for the 90,000 pregnant women who have had the vaccine in the USA.
It is safe to have the vaccine if you are breastfeeding.
For more information, please see the Royal College of Obstetricians and Gynaecologists.
There is no evidence that the vaccine will affect your chances of becoming pregnant. There is no evidence that the COVID-19 vaccine will make you infertile. This is backed by the Royal College of Obstetricians and Gynaecologists, the Association of Reproductive and Clinical Scientists and the British Fertility Society.
The British Fertility Society says if you are trying for a baby or thinking about having a baby in future, you should have your COVID-19 vaccine when it is your turn. You can have the vaccine if you are having fertility treatment. Your medical team will be able to advise you about the best time to have the vaccination during your treatment to avoid having any side effects at the same time as procedures such as egg collection.
The only reason to delay your fertility treatment until after you have had the vaccine is if you want to be protected from COVID-19 before you become pregnant.
Delays can affect your chances of success once you are older than 37.
Three vaccines have now been approved in the UK: Pfizer-BioNTech, Oxford AstraZeneca, and Moderna.
Currently the Pfizer-BioNTech and Oxford AstraZeneca vaccines are being administered, with doses of the Moderna vaccine expected in Spring. These vaccines have unique characteristics which influence when and how they are administered; for instance the Pfizer-BioNTech vaccine must be kept at much lower temperatures than the others.
No. The vaccine administered at each appointment will be influenced by the national distribution pattern, the facilities at each vaccination site and the supply currently available.
If it is your second dose it will be the same vaccine as the first.
Each vaccination site has been carefully selected against a set of comprehensive criteria which ensure that social distancing can be maintained the site is easy to access and the one way systems can be maintained where needed.
We have only selected sites where we are able to comply with government guidance to ensure that each vaccination is administered safely.
People who are unwell should wait until they are fully recovered before having the vaccine. Appointments can be rearranged by contacting your GP or using the national booking service.
If you have symptoms of COVID-19, do not attend your appointment. Please self-isolate and book a test as soon as possible.
The vaccines do not contain common allergens like eggs, shellfish and penicillin.
If you have a history of severe allergies resulting in anaphylaxis, you should talk to your doctor or vaccination team. Some people with allergies may be advised to have a different COVID-19 vaccine or asked to go to a special place where they can be looked after if they have a reaction.
For that latest information about the vaccination programme, please visit the NHS website.
< Back to all news stories